Possible paths of pesticide to people and the
health risk
Rider University, New Jersey
1. The colon cancer cluster following
the waterways of the Mississippi River
Mississippi
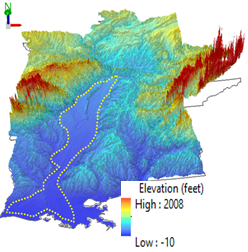
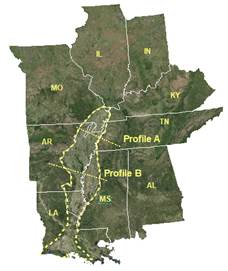
river (MSR) floodplain here refers to the flat alluvial regions in the MSR
basin (Figure 1a), and Mississippi embayment (ME) to the main section of the
MSR floodplain north of the Mississippi River delta (Figure 1b). It has been
known that there is a high colorectal cancer (CC) prevalence in the MSR region (ACS
2018; Lansdorp-Vogellar et al. 2015).
|
Figure 1.
a), elevation (vertically exaggerated) and b), satellite maps showing the
regional landscape patterns of the Mississippi River (MSR) floodplain (dash
line) and Mississippi embayment (ME) alluvial region (north part of the MSR
floodplain before the delta, cutting off by white solid lines between LA and
MS) and locations of two cross-section profile lines. Note the flat landscape
in the MSR floodplain. |
|
|
|
|
Colorectal
cancer (CRC) is the second deadliest cancer worldwide (2017/s data)
and the third deadliest cancer in the US in 2016 (CCS 2018; ACS 2018). There
was an annual average of 44,089 deaths for CC, and 6,562 deaths for rectal
cancer (RC) between 1999 and 2016 in the US alone based upon the database of
the US Centers for Disease Control and Prevention (CDC, https://wonder.cdc.gov).
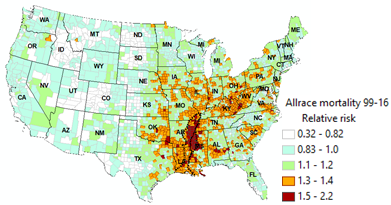
There is an apparent colon cancer cluster along the waterways of the
Mississippi River tributaries for data of both all races and white only
population. Risk level of colorectal cancer incidence in 86 counties of
Mississippi River floodplain was about 29 % higher than that of other counties
in the 48 contiguous states. Risk ratio of colon cancer mortality in 63
counties of Mississippi embayment was 33 % higher than that of other counties
in the 48 states between 1999 and 2016. Risk ratios of colorectal cancer
incidence and colon cancer mortality in Mississippi River floodplain are higher
after smoking and diabetes factors were filtered off.
|
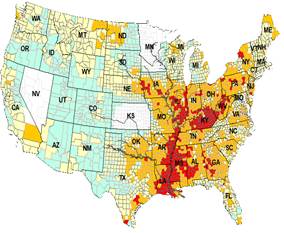
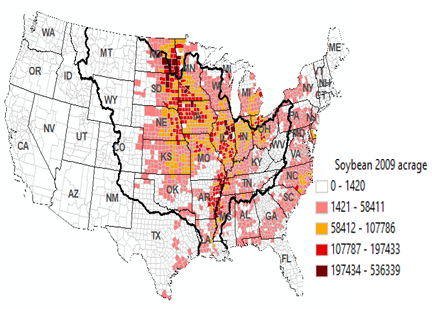
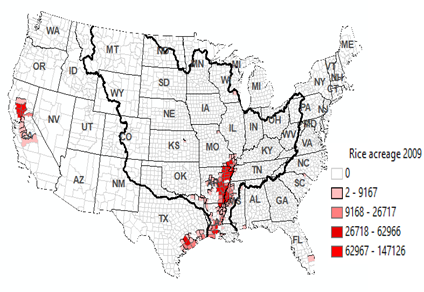
Figure 2.Colon cancer cluster following the waterways of the Mississippi
River. a)-d), Spatial patterns of CRC incidence (2011-2015) , CC mortality
(1999-2016) relative risk, e), soybean and f), rice acreage in 2009 in the 48
US states. MSR flood plain is outlined by dash line in a) and Mississippi
embayment (ME) region is outlined by solid line in b). They are the same
lines shown in satellite map in Figure 1. e), isopleth map of generalized
colon cancer mortality rates (CCMR, 3 cell average), Colorectal (CRC) data
are from US Centers for Disease Control and Prevention. |
|
|
|
|
|
|
|
|
|
|
|
CCMR: colorectal cancer mortality rate
deaths/100,000 people |
|
2. Possible causes of this colon
cancer cluster in the Mississippi River floodplain.
1). Pesticide is
likely the most prominent factor affecting the colon cancer cluster in the
Mississippi River floodplain
Area of high
CRC incidence risk in the MSR region roughly follows the waterways in the MSR
floodplain except for the two states (KY and WV) with high smoking rates and
the two states (MS and AL) with high diabetes prevalence (Figures 1, 2). This
is also apparent in the white population only plots. There is a progressive
increase of CC risks with decreasing distance to the MSR floodplain, ME region
and the Holocene alluvial part of the MSR floodplain in the 48 states (Figures
2, 3, 4).
|
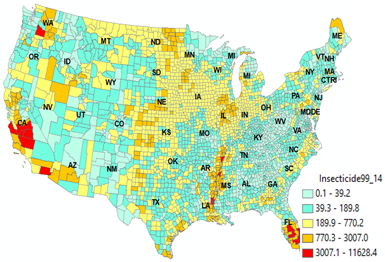
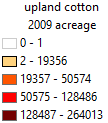
Figure 3. a). Annual total pesticide application is counties of the US
between 1999 and 2014 in Kg (Raw data were from USGS
national sysnthesis project). b), soybean, c), rice acreage
and uland acreage in 2009 in the 48 US states. Thick zigzag lines in b) show
the boundary of the Mississippi River (MSR) floodplain. Main stream branches
of the MSR are shown in a). Note the runoff water concentrate the pesticide
runoff from corn and soybean field into the Mississippi River floodplain.
Thick zigzag lines in b) show the boundary of the MSR basin. Main stream
branches of the MSR are shown in c) and d). Crop acreage data are from US
Department of Agriculture Farm Service Agency (USDA FSA) that collected data
from farm producers who participated in the program (USDA FSA 2018). Crop
acreage here is used as a proxy of the various pesticide usuage in the
region. |
|
|
a). |
|
|
|
|
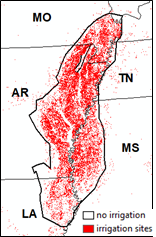
About 80 %
of the US corn and soybeans, and much of the cotton, rice, sorghum and wheat
are produced in the MSR basin (area outlined by the MSR basin line in Figure
2f, e of later section) because of the suitable climate and soil conditions
(Goolsby and Pereira 1995).
Mississippi
River basin produces about 80 % of major US crops and has about two-thirds of
US pesticides used for agriculture. It is probably the most pesticide polluted
river in the US
(Garbarino et al. 1995; Gianessi and Puffer 1991; Goolsby and Pereira 1996;
Tiryaki and Temur 2010). High clay contents in the Holocene alluvium area of
the ME region can adsorb more pesticides and extend the duration of pesticides
in this area (Kingsbury et al. 2014) . Heavy irrigation and long history of
pesticide application result in extensive pesticide pollution in both surface
and ground water in the low lying MSR floodplain (Bouman et al 2002; Castaneda et al.
1996). The particularly high spatial coincidence between high CC risk
and high water irrigation of the rice-upland cotton strip (~56 % of US rice,
~27 % of US upland cotton) in the Mississippi embayment region implies a
possible association of water pollution-pesticide application with high CC
risk. Crop acreages here are used as proxies of the various pesticide application.
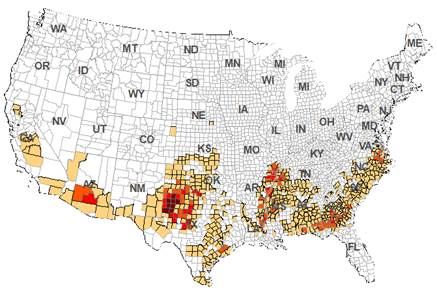
2). Smoking and diabetes rates are
the other likely factors affecting the cluster formation
Previous
studies suggested that cigarette smoking is associated with an increasing risk
of CRC (Botteri et al. 2008; Cheng et al. 2015; Liang et al. 2009; Marley and
Nan 2016). This is consistent with the significant correlations between smoking
and higher CRC incidence risk (r=0.55, p=0.00) and CC mortality rates (r=0.57,
p=0.00) shown in this study (Figure 4). Kentucky and West Virginia have the
highest smoking prevalence rates in the US and they also have higher CRC and CC
risks than surrounding states. Increase of RRs for CC after smoking factor
being filtered off indicates an independent association of CC risk and
pesticide (Table 1). In addition, several epidemiological and experimental
studies have reported a strong linkage between type II diabetes and exposure to
some pesticides such as organochlorine and organophosphate pesticides
(Juntarawijit and Juntarawijit 2018; Lee et al. 2007; Park et al. 2019).
Organochlorine and organophosphates have been suspected to affect glucose
metabolism by blocking cholinesterase activity, oxidative stress, nitrosative
stress, physiological stress, adrenal stimulation, and inhibition of
paraoxonase (Evangelou et al. 2016; Juntarawijit and Juntarawijit 2018).
Connection between CRC risk and diabetes has also been established. CRC risk
was reported to be 27% higher in patients with type II diabetes than in
non-diabetic controls (Gonzalez et al. 2017). The idea is that abnormally high
levels of insulin (hyperinsulinemia) and glucose create an environment in the
colon that can damage the mucosa, or lining of the colon and promotes the
development and growth of CC. The significant correlation (r=0.54, p=0.00) and
striking geographical coincidences between geographical distributions of high
CC mortality and diabetes (particularly AL, GA, SC, NC and VA in Figure 4) and
regions of upland cotton where there were intensive insecticide applications
corroborate this association of pesticide, diabetes and CC risk (Figure 4).
However, higher RRs for smoking filtered CC data (RR, 1.61, 95%CI: 1.55-1.66)
and diabetes filtered CC data (RR, 1.45, 95%CI: 1.42-1.47) than their
corresponding pre-smoking and diabetes filtered RRs also indicate exposure to
pesticide being a possible independent CC risk factor.
|
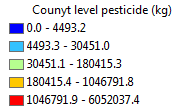
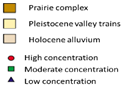
Figure 4. Choropleth maps of a), smoking and b), diabetes prevalences.
The likely high colorectal caner concentrations in Kentucky and West Virginia
are likely related to high smoking prevalence in two states. High colorectal
cancer rates in AL, GA, SC and NC are likely related to diabetes prevalences
in these states. Also notice the diabetes prevalence region is also the
region of concentrated upland cotton fields. Diabetes are reported to be
related to pesticide application, particularly organochlirne and
organophosphate. Diabetes region is also coincided with the high proportion
of black population. |
|
|
|
|
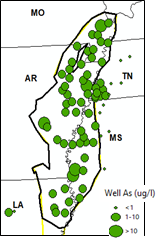
Another
environmental toxin that might facilitate CC risk in the MSR floodplain is the
high arsenic level in both soil and water of the Mississippi embayment region
(Figure 5, Pillai et al. 2010). High arsenic levels in anoxic soil condition of
this region facilitate the release of the bioavailable arsenic to plants and
well water (Kingsbury et al. 2014; Kleiss 2000). The release of bioavailable
arsenic can be evidenced by the high arsenic level in long-grain rice of the US
at 0.26 ug As g-1, the highest among data from worldwide samples
reported by Williams et al. (2005). High arsenic intake was reported to be
associated with variety of cancers, including lung, kidney and colon, though
arsenic in organic form can be less toxic than in inorganic form (Garcia-Esquinas et
al. 2013; Martinez et al. 2011; Smith1 et al. 1992; Yang et
al. 2008). Therefore, possible high arsenic exposure in the ME region can be a
concern as well.
3). Zoomed in on Mississippi
Embayment region
High
pesticide runoff from upstream was concentrated in the Mississippi River
floodplain with levee over breach. The fine sediment, rich organic and high
moisture retains pesticide and keep them from decomposing.
High
pesticide application-and low land elevation--- high pesticide in water--- high
pesticide in fish---high colorectal cancer (CRC).
|
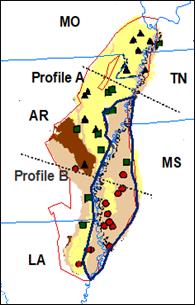
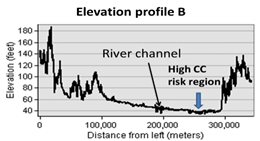
Figure 5. a), Herbicide detections
in water; b), DDT in fish tissue in the Mississippi embayment (ME) between
1997-1998 (Modified from Kleiss et al. 2000); c), zoomed in high CC incidence
risk around the ME between AR and MS; d) and e), elevation profiles crossing
the MSR flood plain. Holocene alluvium region is indicated by color legend in
a) and b). |
|||
|
a) High herbicides in water |
b) high DDT in fish |
c) High CRC risk of all races |
|
|
|
|
||
|
|
|
||
High
pesticide application-and low land elevation--- high pesticide in water--- high
pesticide in fish---high colorectal cancer (CRC)
|
Figure
6. a), agricultural irrigation sites in the Mississippi River Basin (2012,
data from USGS Irrigation, 2018); b), higher arsenic concentrations measured
in well water in the ME region (Data from Kingsbury et al. 2014); c) zoomed in mortality risk map of white population in ME region. |
||
|
a) Abundant irrigation sites |
b) high arsenic in water |
c) high white CC mortality risk |
|
|
||
3. Colon cancer risk in the Mississippi
River floodplain is above 30% higher than that in rest of the 48 conterminous
US states
Rate (colorectal cancer) ratios values of 1.29 (95%CI,
1.26-1.33) for CRC incidence and 1.33 (95%CI, 1.3-1.31) for CC mortality in the
MSR region to the rest of the 48 states indicate the significant CRC and CC
risks in the MSR floodplain, particularly the Holocene alluvial area of the
floodplain (Figures 5 and 6, Table 1). Though diabetes filtered RRs of CRC
incidence and CC mortality are only slightly higher than their pre-filtered
levels, smoking filtered RRs of CRC incidence and CC mortality rates are
significantly higher than their corresponding pre-filtered RRs in the ME region
and the overall MSR floodplain (Table 1).
Table 1. Risk ratios
(RR) of CRC Incidence and CC mortality of counties in the Mississippi River
region to that of other counties in the 48 contiguous US states
|
Risk Ratios (RR) |
lower 95% RR |
Upper 95% RR |
|
|
Risk Ratios (RR) |
lower 95% RR |
Upper 95% RR |
|
|
CRC
Incidence-Mississippi River floodplain |
CC
Mortality-Mississippi embayment area |
|||||||
|
All races, sexes |
1.29 |
1.26 |
1.33 |
All races, sexes |
1.33 |
1.3 |
1.37 |
|
|
white, all sexes |
1.22 |
1.17 |
1.29 |
white, all sexes |
1.21 |
1.16 |
1.25 |
|
|
all races, male |
1.29 |
1.23 |
1.34 |
all races, male |
1.38 |
1.33 |
1.43 |
|
|
all races, female |
1.22 |
1.17 |
1.27 |
all races, female |
1.28 |
1.23 |
1.33 |
|
|
CRC
Incidence-Mississippi embayment area |
CC Mortality-Holocene
alluvial area |
|||||||
|
All races, sexes |
1.26 |
1.22 |
1.31 |
All races, sexes |
1.43 |
1.39 |
1.47 |
|
|
white, all sexes |
1.22 |
1.2 |
1.24 |
white, all sexes |
1.16 |
1.11 |
1.21 |
|
|
all races, male |
1.23 |
1.18 |
1.31 |
all races, male |
1.50 |
1.44 |
1.56 |
|
|
all races, female |
1.17 |
1.1 |
1.23 |
all races, female |
1.43 |
1.37 |
1.49 |
|
|
Smoking filtered CRC incidence and CC mortality, Mississippi embayment (ME) and
Mississippi River floodplain (MSR) |
Diabetes filtered CRC incidence and CC mortality, Mississippi embayment (ME) and Mississippi
River floodplain (MSR) |
|||||||
|
All races, sexes-CRC-MSR |
1.38 |
1.36 |
1.40 |
All races, sexes-CRC-MSR |
1.32 |
1.30 |
1.34 |
|
|
All races, sexes-CRC-ME |
1.31 |
1.29 |
1.34 |
All races, sexes-CRC-ME |
1.26 |
1.24 |
1.28 |
|
|
All races, sexes-CC-MSR |
1.46 |
1.42 |
1.56 |
All races, sexes-CC-MSR |
1.36 |
1.34 |
1.38 |
|
|
All races, sexes-CC-ME |
1.61 |
1.56 |
1.66 |
All races, sexes-CC-ME |
1.45 |
1.42 |
1.47 |
|
Note: For the
risk ratio calculation, counties in the Mississippi River floodplain or
Mississippi embayment area or Holocene alluvial area were considered as exposed
area while counties outside these areas were considered non-exposed areas (see
Figures 1, 2and 4 for geographical location).
4. Pathways of pesticide to people
DDT is likely still in your blood today -
and you are right, it was banned in 1972 in the US! Metabolites of some
pesticides can really last.
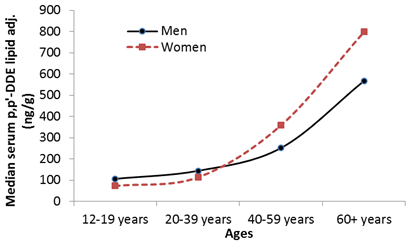
Various
pesticide metabolites found in high percentage (>80 %) of NHANES studies
including those from farming states, indicates the rampant exposure of general
population to pesticide and persistence of some pesticides in nature and their
ability to accumulate in human body (Barr et al. 2005; Jablonowski et al. 2011; Jaga and Dharmani
2003). Even though DDT was discontinued in 1972 in the US, DDT and its
metabolite still found ways to accumulate in fish (Figure 5) and in fat tissues
of people in NHANES surveyed population (Figure 7).
|
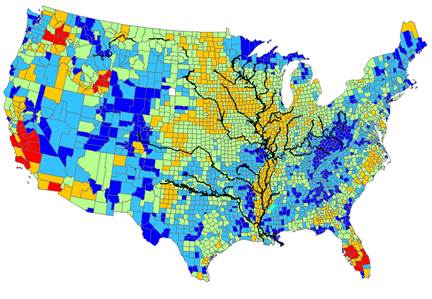
Figure 7.
a), concentrations of p,p/-DDE, a metabolite of DDT between 2003
and 2014 in serum samples of 1781 men and 1903
women vs. age; b),
trend of insecticide application vs. trends of CC incidence and CRC mortality
rates in US. |
|
|
|
|
It is generally
agreed that people from agricultural region have higher exposure to pesticides
than people from non-agricultural region (Huen et al. 2012; Morgan et al. 2008).
There are multiple sources and pathways for people to be exposed to pesticide,
including pesticide dust, residues in water and food (Morgan et al. 2008).
Given that
both surface and ground water in the MSR flood plain are probably the most
pesticide polluted water historically, it is likely that long-term low-dose
exposure to pesticide residues in drinking water is one of the most important
pathways of pesticide to people. Results from previous studies and analyses of
the USDA PDP drinking water project data in this study have shown that many
public water treatment facilities are not very effective at removing pesticide
residues (Donald et al. 2007; Stackelberg et al. 2007; USDA PDP-DWP 2018). It is
reported that individual herbicide removal rates in finished drinking water
varied from 16 % to 84 % (with 6.4 herbicides measured on average) in northern
Great Plains (Donald et al. 2007). Though switching from the surface water to
groundwater can alleviate levels of pesticide residues in the water supplies,
trace amount of pesticide still exists in many water wells (USDA PDP-DWP 2018).
Results of
previous epidemiology studies on the association of the highest mortality rates
(1950-1989) in the US for several cancers, including CC with usage of the
Mississippi River as a source of potable water in Louisiana support the
argument of a possible association between water pollution and CC risk (Cantor
1997; Goitlieb et al. 1982; Page 1976).
The second
likely pathway of pesticide to people is food consumption. Residues of
pesticides are reported in 78 % to 85 % of fruits, vegetables and grains (USDA
2015, 2016). Cyclic changes of urinary pesticide levels in the same group of
people after switching from inorganic to organic food and then from organic to
inorganic food in an experiment study indicates that food consumption can be a
significant pathway of pesticides to people, and maybe the most significant
pathway to people in non-agricultural regions (Lu et al. 2006). Given that up
to 80 % of the food supplies in the 48 contiguous US states, other than a few
coastal states, could be local (within 100 miles of production, Zumkehr and
Campbell 2015), exposure to pesticide from consumption of local food supplies
can be a major source of exposure for people in the MSR floodplain (Holme et al. 2016).
Exposure to pesticide
fume and dust can be an important pathway of pesticide to people in
agricultural regions (Morgan et al. 2008). However, whether respiration intake
is a valid pathway of pesticide that can affect colon in the general public is
not certain and it is evidenced by the inconsistent result of agricultural
cohort studies (Lee et al. 2007; Weichenthal et al 2010). In addition,
adsorptions of pesticide fume and dust by people might be similar to adsorption
of mercury vapor by people, where lung and kidney have the most accumulation,
instead of colon (Asano et al. 2000; Lien et al. 1983; Ye et al. 2013). More
studies are needed in this aspect.
Studies are
needed to identify the types of pesticides that are prone to rise colon cancer
risk.
5. Living in the high colorectal
cancer risk area of the Mississippi River Floodplain, what can you do?
Counties in
the flood plain of the five states including southern corner of Missouri, east
part of Arkansas, Louisiana, west parts of Tennessee and Mississippi states are
the most vulnerable counties that are susceptible to elevated pesticide
affected colorectal cancer risk (Figures 1 and 2).
Filtering
water and enhance the removal of the pesticides--- improvement in quality of
both public water and private water treatment can help reduce the exposure.
More organic food can also help reduce the risk.
-----------------------------------------------------
References
Asano, S., K. Eto, E. Kurisaki, H. Gunji,
K. Hiraiwa, M. Sato, H. Sato, M. Hasuike, N. Hagiwara and H. Wakasa. 2000.
Acute Inorganic Mercury Vapor Inhalation Poisoning. Pathology International 50(3):169-74. doi: 10.1046/j.1440-1827.2000.01032
Barr, D.B., R. Allen, A.O. Olsson, R. Bravo R, L.M.
Caltabiano, A. Montesano, J. Nguyen, S. et al. 2005. Concentrations
of Selective Metabolites of Organophosphorus Pesticides in the United States
Population. Environmental Research
99(3):314-26.
doi: 10.1016/j.envres.2005.03.012
Besag J.,
J.C. York and A. Mollie. 1991. Bayesian Image Restoration, With Two
Applications in Spatial Statistics (With Discussion). Annals of the Institute of Statistical Mathematics 43:1-20.doi: 10.1007/BF00116466.
Botteri, E., S. Iodice, V. Bagnardi, S.
Raimondi, A.B. Lowenfels and P. Maisonneuve. 2008. Smoking and Colorectal
Cancer: A Meta-Analysis. JAMA
300(23):2765-2778. doi:10.1001/jama.2008.839
Bouman, B.A.M., A.R. Castaneda and S.I. Bhuiyan. 2002.
Nitrate and Pesticide Contamination of Groundwater under Rice-Based Cropping
Systems: Past and Current Evidence from the Philippines. Agriculture, Ecosystems & Environment 92(2-3):185-199. doi:10.1016/S0167-8809(01)00297-3.
Cantor, K.P.
1997. Drinking Water and Cancer. Cancer
Causes & Control 8(3):292-308.
Castaneda, A.R. and S.I. Bhuiyan. 1996. Groundwater
Contamination by Rice Field Pesticides and Some Influencing Factors. Journal of Environmental Science &
Health Part A 31(1): 83-99. doi:10.1080/10934529609376345
CDC
Wonder. 2019. Accessible at https://wonder.cdc.gov/. Accessed 10 March 2019.
CCS
(Colon cancer stats). Key Statistics for Colorectal Cancer. 2018. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. Accessed 4 September 2018.
Cheng J., Y. Chen, X. Wang, J. Wang,
Z. Yan, G. Gong, G. Li, and C. Li. 2015. Meta-Analysis of
Prospective Cohort Studies of Cigarette Smoking and the Incidence of Colon and
Rectal Cancers. European Journal of
Cancer Prevention 24(1):6-15. doi: 10.1097/CEJ.0000000000000011.
Das, V., J. Kalita and M. Pal. 2017. Predictive
and Prognostic Biomarkers in Colorectal Cancer: A Systematic Review of Recent
Advances and Challenges. Biomedicine
& Pharmacotherapy 87:8-19. doi:10.1016/j.biopha.2016.12.064
DeRouen, T.A., and J.E. Diem. 1977.
Relationships between Cancer Mortality in Louisiana Drinking-Water Source and
Other Possible Causative Agents. In Origins
of Human Cancer, edited by H.H. Hiatt, J.S. Watson and J. A.
Winsten, 331-345. Cold Spring Harbor: Cold Spring Harbor Laboratory.
Donald, D.B., A.J. Cessna and N.E.G. Sverko.
2007. Pesticides in Surface Drinking-Water Supplies of the Northern
Great Plains. Environmental Health
Perspectives 115(8):1183-91. doi:10.1289/ehp.9435
Evangelou,
E., G. Ntritsos, M. Chondrogiorgi, F.K. Kavvoura, A.F. Hernandez, E.E. Ntzani
and I. Tzoulaki. 2016. Exposure to Pesticides and Diabetes: A Systematic Review
and Meta-Analysis. Environment
International 91:60-8. doi: 10.1016/j.envint.2016.02.013
Everett,
C.J., and E.M. Matheson. 2018. Pesticide Exposure and Diabetes. Reference Module in Earth Systems and
Environmental Sciences, 407-11.
doi:10.1016/B978-0-12-409548-9.10647-5
Fay, M.P. 1999. Approximate Confidence
Intervals for Rate Ratios from Directly Standardized Rates with Sparse Data. Communications in Statistics - Theory and
Methods 28(9): 2141-2160. doi:10.1080/03610929908832411
Fernandez-Cornejo. J., R.F. Nehring, C.
Osteen, S. Wechsler S, A. Martin and A. Vialou. 2014. Pesticide Use in US Agriculture: 21 Selected Crops, 1960-2008. EIB
124, United States Department of Agriculture
Freeman, L.E.B., J.A. Rusiecki, J.A.
Hoppin, J.H. Lubin, S. Koutros, G. and reotti, S.H. Zahm, C.J. Hines, J.B.
Coble, F. Barone-Adesi, and J. Sloan. 2011. Atrazine and Cancer Incidence Among
Pesticide Applicators in the Agricultural Health Study (1994-2007). Environmental Health Perspectives
119(9):1253-1259. doi: 10.1289/ehp.1103561.
Garbarino, J.R., H. Hayes, D. Roth, R.
Antweider, T.I. Brinton and H. Taylor. 1995. Heavy Metals in the Mississippi
River. in Contaminants in the Mississippi
River, edited by Robert H. Meade, 53-72. US Geological Survey Circular 1133. Denver: USGS.
Garcia-Esquinas, E., M. Pollan, J.G. Umans, K.A.
Francesconi, W. Goessler, E. Guallar, B. Howard, J. Farley, L.G. Best, and A.
Navas-Acien. 2013. Arsenic Exposure and Cancer Mortality in A US-Based
Prospective Cohort: The Strong Heart Study. Cancer
Epidemiology and Prevention Biomarkers, 22(11):1944-1953. doi: 10.1158/1055-9965.EPI-13-0234-T.
Gianessi, L.P. and C. Puffer. 1991. Herbicide Use in the United States. Resources for the Future, Washington,
D.C., USA.
Gilliom, R. J. 2007. Pesticides in U.S. Streams and
Groundwater. Environmental Science
& Technology 41:3407-3413. DOI: 10.1021/es072531u
Goitlieb, M.S., J.K. Carr and J.R. Clarkson. 1982.
Drinking Water and Cancer in Louisiana: A Retrospective Mortality Study. American Journal of Epidemiology
116(4):652-67. doi:10.1093/oxfordjournals.aje.a113448
Gonzalez,
N., I. Prieto, L. del Puerto-Nevado, S. Portal-Nunez, J.A. Ardura, M. Corton,
B. Fernandez-Fernandez, O. Aguilera, C. Gomez-Guerrero, S. Mas and J. A.Moreno.
2017. 2017 Update on the Relationship between Diabetes and Colorectal Cancer:
Epidemiology, Potential Molecular Mechanisms and Therapeutic Implications. Oncotarget 8:18456-18485.
doi: 10.18632/oncotarget.14472.
Goolsby, D.A. and W.E. Pereira.
1996. Pesticides in the Mississippi river. US
Geological Survey Circular 87-102.
Gottlieb, M.S., J.K. Carr, J.K. CARR and
D.T. Morriess. 1981. Cancer and Drinking Water in Louisiana: Colon and Rectum. International Journal of Epidemiology
10:117-126. doi:10.1093/ije/10.2.117
USGS irrigation. 2018. Moderate
Resolution Imaging Spectroradiometer (MODIS) Irrigated Agriculture Dataset for
the United States (MIrAD-US). https://earlywarning.usgs.gov/USirrigation. Accessed 1 March /2019.
Guyton, K.Z., D. Loomis, Y. Grosse, F. El
Ghissassi, L. Benbrahim-Tallaa, N. Guha, C. Scoccianti, H. Mattock and K. Straif.
2015. Carcinogenicity of Tetrachlorvinphos, Parathion, Malathion, Diazinon, and
Glyphosate. The Lancet Oncology
16(5):490-491. doi: 10.1016/S1470-2045(15)70134-8.
Haggar, F.A. and R.P. Boushey. 2009.
Colorectal Cancer Epidemiology: Incidence, Mortality, Survival, and Risk
Factors. Clinics in Colon and Rectal
Surgery 22(4):191-197. doi: 10.1055/s-0029-1242458.
Hansell, A.L., R.E. Ghosh, D. Fecht, and
L. Fortunato. 2014. The Environment and
Health Atlas for England and Wales. Oxford University Press, USA.
Holme, F., B.Thompson, S. Holte, E.M.
Vigoren, N. Espinoza, A. Ulrich, W. Griffith and E.M. Faustman. 2016. The Role
of Diet in Children/s Exposure to Organophosphate Pesticides. Environmental Research 147:133-140. doi:
10.1016/j.envres.2016.02.003.
Huen, K., A. Bradman, K.
Harley, P. Yousefi, D.B. Barr, B. Eskenazi and N. Holland. 2012.
Organophosphate Pesticide Levels in Blood and Urine of Women and Newborns
Living in an Agricultural Community. Environmental
Research 117:8-16. doi: 10.1016/j.envres.2012.05.005.
Jablonowski, N.D., A. Schaffer and P.
Burauel. 2011. Still Present after All These Years: Persistence Plus Potential
Toxicity Raise Questions about the Use of Atrazine. Environmental Science and Pollution Research 18(2):328-331. doi: 10.1007/s11356-010-0431-y.
Jaga, K. and C. Dharmani. 2003. Global
Surveillance of DDT and DDE Levels in Human Tissues. International Journal of Occupational Medicine and Environmental Health
16(1):7-20.
Johnson, C.M., C. Wei, J.E. Ensor, D.J.
Smolenski, C.I.Amos, B. Levin and D.A. Berry. 2013. Meta-Analyses of Colorectal
Cancer Risk Factors. Cancer Causes &
Control 24(6):1207-1222. doi: 10.1007/s10552-013-0201-5
Juntarawijit, C. and Y. Juntarawijit. 2018. Association
between Diabetes and Pesticides: A Case-Control Study among Thai Farmers. Environmental Health and Preventive Medicine
23(1):3. doi:
10.1186/s12199-018-0692-5.
Kingsbury, J.A., J.R. Barlow, B.G. Katz,
H.L. Welch, R.W. Tollett and L. Fahlquist. 2014. Water Quality in the
Mississippi Embayment--Texas Coastal Uplands Aquifer System and Mississippi
River Valley Alluvial Aquifer, South-central United States, 1994--2008. US
Department of the Interior, US Geological Survey.
Kleiss, B.A. 2000. Water Quality in the
Mississippi Embayment, Mississippi, Louisiana, Arkansas, Missouri, Tennessee,
and Kentucky, 1995-98. US Geological Survey.
Lansdorp-Vogelaar, I., S.L. Goede, J. Ma,
W. Xiau-Cheng, K. Pawlish, M. van Ballegooijen and A. Jemal. 2015. State
Disparities in Colorectal Cancer Rates: Contributions of Risk Factors,
Screening, and Survival Differences. Cancer
121(20):3676-83. doi: 10.1002/cncr.29561.
Lee, W.J., D.P., Sandler, A. Blair, C.
Samanic, A.J. Cross and M.C. Alavanja. 2007. Pesticide Use and Colorectal
Cancer Risk in the Agricultural Health Study. International Journal of Cancer 121(2):339-346. doi: 10.1002/ijc.22635
Liang, P.S.,
T.Y. Chen and E. Giovannucci. 2009. Cigarette Smoking and Colorectal Cancer
Incidence and Mortality: Systematic Review and Meta‐Analysis. International Journal of Cancer 124(10):2406-15. doi:
10.1002/ijc.24191.
Lien, D.C., D.N. Todoruk, H.R. Rajani,
D.A. Cook, F.A. Herbert. 1983. Accidental Inhalation of Mercury Vapour:
Respiratory and Toxicologic Consequences. Canadian
Medical Association Journal 129(6):591.
Lu, C., K.Toepel, R. Irish, R.A. Fenske,
D.B. Barr and R. Bravo. 2006. Organic Diets Significantly Lower Children/s
Dietary Exposure to Organophosphorus Pesticides. Environmental Health Perspectives 114(2):260-3. doi: 10.1289/ehp.8418.
Marley, A.R.
and H. Nan. 2016. Epidemiology of Colorectal Cancer. International Journal of Molecular Epidemiology and Genetics
7(3):105.
Martinez, V.D., E.A. Vucic, D.D.
Becker-Santos, L. Gil and W.L. Lam. 2011. Arsenic Exposure and the Induction of
Human Cancers. Journal of
Toxicology 2011:1-14. doi: 10.1155/2011/431287.
Moraga, P.
2017. SpatialEpiApp: A Shiny Web Application for the Analysis of Spatial and
Spatio-Temporal Disease Data. Spatial and
Spatio-temporal Epidemiology 23:47-57. doi:10.1016/j.sste.2017.08.001
Morgan, M.K., L.S. Sheldon, K.W. Thomas,
P.P. Egeghy, C.W. Croghan, P.A. Jones, J.C. Chuang and N.K. Wilson. 2008. Adult
and Children/s Exposure to 2, 4-D from Multiple Sources and
Pathways. Journal of Exposure Science and
Environmental Epidemiology 18(5):486-494. doi: 10.1038/sj.jes.7500641.
Page, T., R.H. Harris and S.S. Epstein. 1976. Drinking
Water and Cancer Mortality in Louisiana. Science 193(4247):55-57.
Park, S., S.K. Kim, J.Y., Kim, K. Lee,
J.R. Choi, S.J. Chang, C.H. Chung, K.S. Park,S.S. Oh and S.B. Koh. .2019.
Exposure to Pesticides and the Prevalence of Diabetes in A Rural Population in
Korea. NeuroToxicology 70:12-8.
doi:
10.1016/j.neuro.2018.10.007.
Peeters, P.J, M.T. Bazelier, H.G. Leufkens, F. de Vries
and M.L. De Bruin. 2015. The Risk of Colorectal Cancer in Patients with Type 2
Diabetes: Associations with Treatment Stage and Obesity. Diabetes Care 38(3):495-502. doi: 10.2337/dc14-1175.
Pillai, T.R., W. Yan, H.A. Agrama,
W.D. James, A.M. Ibrahim, A.M. McClung, T.J. Gentry and R.H. Loeppert. 2010.
Total Grain-Arsenic and Arsenic-Species Concentrations in Diverse Rice
Cultivars under Flooded Conditions. Crop
Science 50(5):2065-2075. doi:10.2135/cropsci2009.10.0568.
Ping, R.
2011. Lifetime Mobility in the United States: 2010, American Community Survey Briefs.
https://www2.census.gov/library/publications/2011/acs/acsbr10-07.pdf. Accessed
4 September 2018.
Samsel, A. and S. Seneff. 2013.
Glyphosate/s Suppression of Cytochrome P450 Enzymes and Amino Acid
Biosynthesis by the Gut Microbiome: Pathways to Modern Diseases. Entropy 15(4):1416-63. doi:10.3390/e15041416
Skrzydlewska, E., A. Stankiewicz, M.
Sulkowska, S. Sulkowski and I. Kasacka. 2001. Antioxidant Status and Lipid
Peroxidation in Colorectal Cancer. Journal
of Toxicology and Environmental Health Part A 64(3)213-222. doi:
10.1080/15287390152543690.
Smith1, A.H., C.
Hopenhayn-Rich, M.N. Bates, H.M. Goeden, I. Hertz-Picciotto, H.M. Duggan, R.
Wood, M.J. Kosnettand and M.T. Smith. 1992. Cancer Risks from
Arsenic in Drinking Water. Environmental
Health Perspectives 97:259-267. doi: 10.1289/ehp.9297259.
Smith2,
D.B., W.F. Cannon, L.G. Woodruff, S. Federico and K.J. Ellefsen. 2014.
Geochemical and Mineralogical Maps for Soils of the Contiguous United States. US Geological Survey Open-File Report,
1082.
Stackelberg, P.E., J. Gibs, E.T. Furlong,
M.T. Meyer, S.D. Zaugg and R.L. Lippincott. 2007. Efficiency of Conventional
Drinking-Water-Treatment Processes in Removal of Pharmaceuticals and Other
Organic Compounds. Science of the Total
Environment 377(2-3):255-272. doi:10.1016/j.scitotenv.2007.01.095
Tiryaki, O.
and C. Temur. 2010. The Fate of Pesticide in the Environment. Journal of Biodiversity and Environmental
Sciences 4(10):29-38.
USDA. 2015, 2016. Pesticide Data
Program. Washington, DC:U.S. Department of Agriculture. Available:
https://www.ams.usda.gov/press-release/usda-releases-2016-annual-pesticide-data-program-summary.
https://www.ams.usda.gov/press-release/usda-releases-2015-annual-pesticide-data-program-summary. Accessed 29 March 2019.
USDA FSA (
Farm Service Agency). 2018. Crop Acreage Data 2007-2017. Accessible at https://www.fsa.usda.gov/news-room/efoia/electronic-reading-room/frequently-requested-information/crop-acreage-data/index. Accessed 29 August 2018.
USDA PDP-DWP
(Pesticide Data Program, Drinking Water Project). 2018. PDP Drinking Water
Project (2001 - 2013). Accessible at
https://www.ams.usda.gov/datasets/pdp/pdpdata.https://www.ams.usda.gov/datasets/pdp/pdp-drinking-water-project.
Accessed 4 September 2018.
USDA-OCE (Office of Chief Economists).
2018. Accessible at https://www.usda.gov/oce/weather/pubs/Other/MWCACP/namerica.htm. Accessed 3 September 2018.
USGS National map. 2018. Small scale
100 meter resolution DEM file. Accessible at https://nationalmap.gov/small_scale/mld/elev100.html. Accessed 29 August 2018.
USGS Irrigation. 2018. Moderate
Resolution Imaging Spectroradiometer (MODIS) Irrigated Agriculture Dataset for
the United States (MIrAD-US). 2002, 2007, 2012 map. Accessible at https://earlywarning.usgs.gov/USirrigation. Accessed 10 March 2019.
Waters, M.D., V.F. Simmon, R. Valencia,
A.D. Mitchell and T.A. Jorgenson. 1980. An Overview of Short‐Term Tests for the Mutagenic and Carcinogenic Potential of
Pesticides. Journal of Environmental
Science & Health Part B 15:867-906. doi: 10.1080/03601238009372221.
Weichenthal, S., C., Moase C and P. Chan.
2010. A Review of Pesticide Exposure and Cancer Incidence in the
Agricultural Health Study Cohort. Environmental
Health Perspectives. 118(8):1117-25. doi: 10.1289/ehp.0901731.
Williams, P.N., A.H. Price, A. Raab, S.A. Hossain, J.
Feldmann, and A.A. Meharg. 2005. Variation in Arsenic Speciation and
Concentration in Paddy Rice Related to Dietary Exposure. Environmental Science & Technology 39(15):5531-5540. doi:
10.1021/es0502324.
Yang, C.Y., C.C. Chang, S.C. Ho and H.F.
Chiu. 2008. Is Colon Cancer Mortality Related to Arsenic Exposure? Journal of Toxicology and Environmental
Health Part A 71(8):533-538. doi: 10.1080/15287390801907509.
Ye, M., J. Beach, J. Martin, and A.
Senthilselvan. 2013. Occupational Pesticide Exposures and Respiratory Health. International Journal of Environmental
Research and Public Health 10(12), 6442-6471. doi:
10.3390/ijerph10126442.
Yu, Z. and C. Lu 2017. Historical
Cropland Expansion and Abandonment in the US During 1850 to 2016. Global Ecology and Biogeography 27(3):
322-33. doi:10.1111/geb.12697
Zhu, L.,
L.W. Pickle and J.B. Pearson. 2016. Confidence Intervals for Rate Ratios
between Geographic Units. International
Journal of Health Geographics 15(1):44:1-13. doi: 10.1186/s12942-016-0073-5.
Zumkehr, A. and J.E. Campbell. 2015. The
Potential for Local Croplands to Meet US Food Demand. Frontiers in Ecology and the Environment 13(5):244-248. doi: 10.1890/140246.
---------------------------------------------------------------------------------------------------------------------------------------
Above contents are extracted from the
work published by Dr. Sun on Sun, H. 2019. Pesticide in the Mississippi
River floodplain and its possible linkage to colon cancer risk, Toxicological
& Environmental Chemistry, DOI: 10.1080/02772248.2019.1604957. If you don/t
want to pay the journal/s page charge to access the article, you can download a full word text
file, click here.
You can also
check out my most recent mesothelioma research here. Sun, H. 2019. North-south
gradient of mesothelioma and asbestos consumption-production in the United
States-Progresses since the 1st asbestos partial ban in 1973. American Journal
of Industrial Medicine. 62(4):337-346. Download a word text file, click
here.
Disclaim: The
project was not financially supported by any agencies. The views here are Dr.
Sun/s personal opinions. They do not represent the views of any
institution or agency. If you have questions regarding your personal health,
consult your physician directly.
Support my research
Considering to support researches in
my laboratory and to make details of this type of research available to the
general public-by supporting the open access publication, so more people can be
aware of the risk posted by the pesticide application in the colon cancer
cluster region and see the evidence. The total
charge for the open access of this article is $2950. The support check and notification email can be sent to Dr. Sun/s
environmental health research, GEMS department, Rider University, 2083
Lawrenceville, New Jersey 08648. Pay to the order: Rider University.
There is an average of 41756 deaths
from colon cancer per year between 1999 and 2017 in the US alone. We want to
make a difference.
My ongoing researches
1). Identification of the types of
pesticide that are more likely to be carcinogenic and potentially responsible
for the colon cancer cluster in the Mississippi River floodplain.
2). Pesticide and all cancer death in
the US.
3). Pesticide impact on Parkinson/s
disease
If you are a researcher or
organization that are interested in collaboration on any of the above projects,
please contact me directly.
Email: hsun@rider.edu,
phone 609-896-5185. Hongbing Sun,
Page updated 5/6/2019.